Adding a Benefits Plan
The Benefits Plan contains plan details such as plan design information. You can add Master Benefit Plans or client-sponsored Benefit Plan data into the individual client workspaces.
Master Benefits Plans are set up and managed in the Admin Workspace on the Benefits Plan dataform. These plans can then be assigned to each client or prospect as offered benefits plans.
Client-Level Benefits Plans are added directly to the prospect or client workspace. This is where you would use a Model Plan to copy a master plan from the Admin Workspace or a plan identified as a Base Plan to a client level plan.
ClientSpace Benefits Plan records equate to “Group Benefit Plans” in the PrismHR application. These plans are the existing plans and plan designs.
To add a Benefits Plan:
- From the modules bar, click
 Workspaces.
Workspaces.
The Workspace Search dashboard opens. - Select the desired workspace and click
 (Open).
(Open).
The Workspace page opens. -
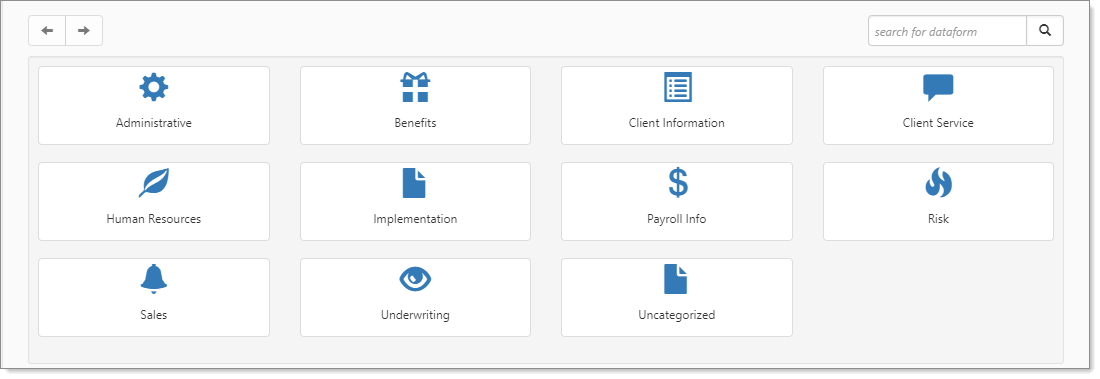
Move down the page to the administrative tiles where you see the dataform categories.
-
Enter "Benefits Plan" in the search for dataform field and then click the Benefits Plan tile.
The Benefits Plan dashboard displays.
-
Click Add.
-
Complete the fields as applicable. Required fields are Model Plan, Carrier Plan Code, Category, Carrier, and Effective Date.
Note:
-
Some values auto-populate from the selected Model Plan. Review the values for accuracy.
-
Fields displayed can vary depending on your configuration as well as the Category (i.e., Health, Vision, Dental, etc.) therefore, all possible fields may not be defined here.
Field Description Model Plan Required. You can select [No Plan Model] for complete manual entry of plan details or pick a plan from the selection list.
The selection list is populated with master plans added to the Admin Workspace and client-level level plans where the Base Plan checkbox is checked on the Benefits Plan record. Pick a Model Plan when you are adding a new client-level plan to copy the plan details from the selected plan to the new plan. This copies the basic plan details, including Plan Title, Carrier Plan Code, Benefit Plan Identifier, Category, Type, Default Rate Group, Effective Date, Expiration Date and more. It also copies over any field values entered in the "Prism Coverage Levels" and "Plan Design" fieldsets.
Product Product category used to identify the companies for which a plan was designed. May auto-populate from the model plan. EX: PEO, HRO, ALL. Plan Title Plan name. The field accepts special characters in the plan name.
Note: Ensure the name is descriptive and follows consistent naming practices as it comprises part of value used in the Benefit Plan field drop-down list. The Benefit Plan field is on the Offered Benefit Plan dataform. The list is sorted by Effective Date and then by Plan Title (i.e., Plan Title within Effective Date), with special characters in the Plan Title being sorted before letters.
Carrier Plan Code Required. Code used by the carrier to identify the plan. If you export to PrismHR, the ClientSpace Carrier Plan Code should match the PrismHR Plan ID field value.
Note: Carrier Plan Code is used in business logic throughout ClientSpace. Examples include:
-
Carrier Plan Code is used in plan dependency business rules (HE_RequirePlanByCategoryType) to require that certain plans are bundled together. See Business Rule Methods.
-
Carrier Plan Code is used in the Client Benefit Plans Export merge procedure where it is evaluated in the current year plan against the renewed plan for a match to determine whether a renewed plan is inserted as an "ADD" Action line item in the Client Benefit Plans Export merge file for the Current Year Plan OR inserted as a "TERM" Action line item in the Client Benefit Plans Export merge file for the Prior Year Plan. See Client Benefit Plans Export.
-
Carrier Plan Code is evaluated by the Set OPB business rule used to set the Offered Benefits Plan field on the Employee Benefits Details form. The rule triggers when you create and save a new Employee Benefit Details record or the Offered Benefit Plan field on an existing Employee Benefit Details record is empty (i.e., blank) and you save the record. For the OBP to be set in the field one of the criteria requires the Employee Benefits Detail form Plan ID to match the parent benefit plan's Carrier Plan Code.
Rate Group Type Rate Group pricing model. Valid options include Banded or Tiered. Select "Tiered" to identify a plan that uses percentage tiers for pricing. Select "Banded" for plans that uses groups or bands (i.e., a demographic factor of age or salary) to determine pricing. Benefit Plan Identifier This is an identifier typically provided by a payroll system administrator. Date Last Renewed Auto-fills with the date the benefits plan was last renewed. This can come from a manual renewal by clicking the Renew link in the Action Center on the plan or through an import of data that is extracted from Prism or other sources. Default Rate Group Default Rate Group for this plan. Only set it on the benefits plan record for health plans that use risk tiers. Otherwise, set the Default Rate Group on the Benefit Batch of the associated OBP. See Setting Default Rate Groups. Category Required. The benefits plan category: Health, Dental, Vision, Life Insurance, Long-Term Disability, Short-Term Disability, Supplemental, Bond, and Other.
Note: If the benefits plan category lookup fields listed above are configured to reference the following Payment Responsibility metadata, ClientSpace will use a business rule to automatically set the Employer Contribution method amount and percent when applicable. See Configuring the Benefit Plan Category Payment Responsibility.
Carrier Required. The company issuing the insurance policy. Type Account type identifier for tax advantaged, employer-offered benefits accounts used to pay for qualified medical expenses such as HRA, FSA, and HSA. Renewed From If the benefits plan is renewed, the orginal plan it was renewed from is identified here. Status benefits plan status. Valid options include New, Pending Activation, Active, Expired, and Cancelled. Group # This number is an identifier assigned by the carrier for the service provider. Plan Dependency Bundle This field is required for use with the HE_RequirePlanDependency business rule method. It is used to select the Plan Dependency flag for each benefits plan that you want to include in a Plan Dependency Bundle. Each plan with the Plan Dependency flag will be required based on the business rule setup.
Plan Description
Free text field for entering a plan description or summary as well as any special notes about the plan.
Effective Date
Required. Plan effective date.
Expiration Date
Plan expiration date.
Gradient AI Benefits Underwriting Group Used to identify health plans that are underwritten as a group. Prism Coverage Levels
On the Benefits Plan dataform, there is a Prism Coverage Levels fieldset. This fieldset allows you to add coverage level names and indicate which coverage levels display (i.e., set field display rules) on the Benefit Plan Manager (BPM) Group Summary and Plan Comparison grids. You can add up to five (5) coverage levels.
By default, if you do not add any coverage level names or set any field display rules, the following coverage levels display for all plans:
-
Employee Only
-
Employee + Spouse
-
Employee + Child(ren)
-
Employee + Family
-
Domestic Partner
See Configuring the Benefits Plan Prism Coverage Levels Fieldset.)
Coverage Details Free text field for entering details about the coverage offered in the plan. This is useful for capturing details that are not recorded in the Plan Design fieldset. Monthly Premium This fieldset holds the base rate for each coverage level.
Note:
-
For plans that use standard rate groups (or what we refer to as manual rate groups in ClientSpace), the benefits plan base rates are optional.
-
For plans that use percentage tiers, the base rates are required because each percentage tier rate group is calculated from the base rate.
EO Cost Base rate for the Employee Only (EO) coverage level. EC Cost Base rate for the Employee + Child(ren) (EC) coverage level. EF Cost Base rate for the Employee + Family (EF) coverage level. ES Cost Base rate for the Employee + Spouse (ES) coverage level. EK Cost Base rate for the Employee + Domestic Partner (EK) coverage level. General Details Referrals Required For Health, Dental or Vision plans: Free text field for entering additional details about the circumstances under which a referral may be required before an insured can receive care (if this was not captured in the Plan Design section.) Out of Network Benefits Available For Health, Dental or Vision plans: Free text field for entering additional details about any out-of-network benefits (if this was not captured in the Plan Design section.) Eligible Age for Dependents For Health, Dental or Vision plans: Enter the age or age range for dependents to be eligible for coverage under this plan. Plan Design Complete the applicable fields, including deductibles, co-pays, and out of pocket maximums as applicable.
Note:
-
Fields vary by benefits plan category.
-
If you use the Benefit Plan Manager (BPM), details entered in the Plan Design fieldset of the Benefits Plan in BPM. See Configuring the Benefits Plan Dataform Plan Design Fieldset.
Additional Info For supplemental plans: Used to specify supplemental plan premium calculation or contribution or describe other details about the coverage.
Note: For supplemental plans, only the information in this field displays in BPM. This is because the contribution and premium amounts are typically calculated using a Premium Basis associated with the benefits plan Category such as per $1,000 of payroll and BPM cannot provide these calculations using the tiered, per person format that it uses for Health, Dental, Vision, and Life (Std/Ltd). BPM does not access payroll data to make these calculations.
Use the Additional Info field to indicate that any premiums or contributions indicated in the plan details are not calculated based on an amount per person. They are amounts per X dollars of payroll. You can also add additional details describing the coverage.
Base Plan When the Base Plan checkbox is checked on a client-level plan, the benefits plan is added to the Model Plan drop-down list on the Benefits Plan dataform.
Note: Master plans from the Admin Workspace as well as other client-level plans flagged as a Base Plan are available in the Model Plan list of plans to copy from when adding a new, client-level plan.
Use in Pricing Comparison Flags the plan for use benefits underwriting and quoting.
Suppress from Presentation
Benefits plan suppression options are used to keep offered plans using this parent benefits plan record from displaying and being included in calculations.
Note:-
A suppressed plan will still be listed as an associated OBP on the Benefits Batch (when you click the Associated OBPs link in the Action Center of the Benefits Batch.)
-
Since suppression options can apply to multiple areas, including the Benefits Renewal Workbook merge, the Benefits Renewal DocuSign Approval merge, and BPM, carefully review the option definitions to ensure you are selecting the correct item.
The following options are available:
-
Suppress From Entire Presentation - Removes this plan from all locations in BPM and from the Benefits Renewal Workbook merge.
-
Suppress From Signature Page Only - Removes this plan only from the Signature Page in BPM and the Benefits Renewal DocuSign Approval merge.
-
Suppress From Plan Selection & Contributions Only - Removes this plan from the Plan Comparison and Summary pages in BPM and from the Benefits Renewal Workbook merge.
Active
Checked indicates an active benefits plan. Unchecked indicates an inactivated or archived benefits plan.
-
-
Click Save to save and close or Apply to save and keep the benefits plan record displayed.